|
Case Report
Acute pancreatitis in a patient with COVID-19: A case report
1 DNB; Postgraduate Student at Institute of Liver Gastroenterology & Pancreatico Biliary Sciences, Sir Ganga Ram Hospital, New Delhi, India
2 MD, DM; Consultant at Institute of Liver Gastroenterology & Pancreatico Biliary Sciences, Sir Ganga Ram Hospital, New Delhi, India
3 MD, DNB, FRCPE; Consultant at Institute of Liver Gastroenterology & Pancreatico Biliary Sciences, Sir Ganga Ram Hospital, New Delhi, India
4 MD, DNB; Consultant at Institute of Liver Gastroenterology & Pancreatico Biliary Sciences, Sir Ganga Ram Hospital, New Delhi, India
5 MD, DM, Chairman at Institute of Liver Gastroenterology & Pancreatico Biliary Sciences, Sir Ganga Ram Hospital, New Delhi, India
Address correspondence to:
Praveen Sharma
Department of Gastroenterology, Sir Ganga Ram Hospital, New Delhi,
India
Message to Corresponding Author
Article ID: 100092Z04MK2020
Access full text article on other devices

Access PDF of article on other devices

How to cite this article
Kolhe M, Sharma P, Anikhindi S, Bansal N, Saachdeva M, Arora A. Acute pancreatitis in a patient with COVID-19: A case report. Int J Hepatobiliary Pancreat Dis 2020;10: 100092Z04MK2020.ABSTRACT
Introduction: The world is in the middle of the COVID-19 global pandemic. Case load is rising on exponential rate and we have already crossed 20 million mark. Typical presenting feature of COVID-19 is asymptomatic/mild or symptoms/acute respiratory illness and death. Gastrointestinal (GI) manifestations are common like loose stools, nausea, and abdominal pain.
Case Report: A case of a 19-year-old girl without previous comorbidities presented with typical symptoms of COVID-19. During hospital stay she developed abdominal pain and diagnosed severe pancreatitis. All common causes of acute pancreatitis were ruled out by doing relevant investigations. Her pancreatitis was severe and required percutaneous drainage of necrotic material. She was discharged after prolonged hospital stay even after her negative COVID test.
Conclusion: Atypical presentation of COVID-19 is increasing with increasing case load. Abdominal pain in a patient with COVID should be evaluated for acute pancreatitis and be treated accordingly to lessen morbidity and mortality.
Keywords: Abdominal pain, Acute pancreatitis, Atypical presentation, COVID
Introduction
At present, the world is going through a pandemic of COVID-19. Typical presentation in majority of COVID-19 patients is characterized by cough, fever, anosmia, lower respiratory tract infection, mild abdominal pain, and loose stools. Fewer patients developed severe respiratory symptoms requiring oxygen supplementation and ventilatory support. As the number of cases is rising, physician is witnessing the atypical presentations of COVID-19 [1],[2]. Patients with COVID-19 and severe abdominal pain diagnosed as acute pancreatitis is a rare presentation [3],[4]. We are reporting a case from COVID-19 who developed severe acute pancreatitis as a complication of illness.
Case Report
19-year-old young female patient with body mass index of 32 kg/m2 presented with fever, anorexia, dry cough, and difficulty in taking deep breath of three days duration. In view of typical symptoms in the present pandemic she was investigated for COVID-19 and found to be COVID-19 positive by real-time qualitative polymerase chain reaction (PCR) for COVID-19 (SARS-COV-2) testing. There was no previous history of diabetes, hypertension, any substance addiction, or sexual promiscuity. She was admitted in view of respiratory symptoms and fever, she was maintaining her oxygen saturation at room air. She was started on oral acetaminophen and multivitamin. She did not receive any antibiotics or any therapy for COVID-19. Later on, day 7 of illness, she developed severe pain in abdomen which was radiating to back associated with nausea and vomiting mimicking pain of acute pancreatitis. She had no past history of acute or chronic pancreatitis. She developed tachycardia, her oxygen saturation remained normal but developed epigastric tenderness. She was started on intravenous (IV) fluids, Pantoprazole, Tramadol, Ondensetron, subcutaneous regular insulin if needed to keep blood sugar under normal range. Her serum lipase and amylase level were high (>500 IU/L) at the time of pain (Table 1). Her routine reports are shown in Table 1.
Her chest X-ray of posteroanterior view showed blunting of cardiophrenic angle on left side, suggestive of pleural effusion. Ultrasonography of abdomen was done which showed no gall bladder calculus, edematous pancreas along with Grade 2 fatty liver with mild splenomegaly was noted. She was continued on conservative management.
On day 13 of hospitalization, her abdominal pain got worsened even on conservative therapy and keeping her nil per orally. She underwent contrast enhanced computed tomography abdominal scan (CECT), which showed acute necrotizing pancreatitis with intrapancreatic necrosis and peripancreatic fluid, inflammatory changes, and phlegmon (Figure 1). She was started on IV antibiotics along with other supportive treatment. Her symptoms were improved over the period of one week. Oral diet was resumed. But on the day 18 of admission she had recurrent fever spike and decrease in oxygen saturation.
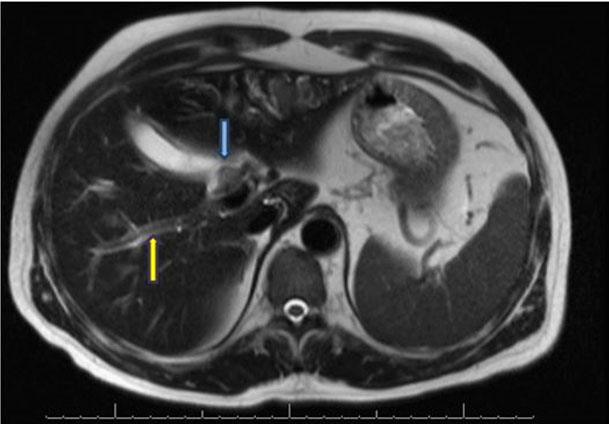
Repeat CECT scan of chest and abdomen was done which showed left sided minimal pleural effusion and underlying collapse of lung. There was evidence of intra- and peri-pancreatic necrotic collections. As compared with previous CT scan, there was organization of collections (Figure 2). Intravenous antibiotics were upgraded and inflammatory markers and blood cultures were sent. On day 19 of illness, she had recurrence of fever. Blood cultures and urine culture were sterile after 48 hours. Repeat real time qualitative PCR was negative for COVID-19 on day 19 of hospital admission. In view of fever and organized collection she underwent ultrasonography guided percutaneous drainage of collection and her fever subsided. She is still under follow-up with drain in situ.
Discussion
This is an unusual presentation of COVID-19 and acute pancreatitis. In this case, we have found that after ruling out other causes of acute pancreatitis, there is a temporal association between acute pancreatitis and COVID-19. Viruses can cause acute pancreatitis which may be indistinguishable from other causes. This patient reported abdominal pain on day 7 of fever and hospital admission. She developed acute pancreatitis which required percutaneous drainage. There are few case reports published recently, which also report association of pancreatitis with COVID-19 [4]. There are wide varieties of infectious agents which can cause acute pancreatitis including viruses viz. mumps, coxsackie, hepatitis B, cytomegalovirus, varicella-zoster virus, herpes simplex virus [5]. Novel corona virus can be potential cause of pancreatitis as it also bears ACE-2 receptors which is entry point for the virus [6].
Though the incidence of COVID-induced pancreatitis is very low but the GI manifestations are rising. One of the first studies from Wuhan, China quoted that GI manifestations are low but later studies from US stated that GI manifestations are much higher than China due to obesity and other metabolic diseases. This study shows that 7.8% patients had abdominal pain [7]. So if the patient has abdominal pain then pancreatitis should be suspected and treated accordingly. We have witnessed the case of acute pancreatitis which had severity of moderately severe course and has caused significant morbidity in patient. So we stress on the fact that while evaluating abdominal pain in COVID patient, acute pancreatitis should be suspected as it can cause prolonged stay and higher morbidity if not diagnosed in time.
Conclusion
Gastrointestinal manifestations of COVID illness are not much frequent. Abdominal pain in COVID patients should be investigated in terms of acute pancreatitis. It will help to diagnose acute pancreatitis in time and reduce its complications, associated morbidity and mortality.
REFERENCES
1.
Baj J, Karakuła-Juchnowicz H, Teresiński G, et al. COVID-19: COVID-19: Specific and non-specific clinical manifestations and symptoms: The current state of knowledge. J Clin Med 2020;9(6):1753. [CrossRef]
[Pubmed]

2.
Tian Y, Rong L, Nian W, He Y. Review article: Gstrointestinal features in COVID-19 and the possibility of faecal transmission. Aliment Pharmacol Ther 2020;51(9):843–51. [CrossRef]
[Pubmed]

3.
Hadi A, Werge M, Kristiansen KT, et al. Coronavirus Disease-19 (COVID-19) associated with severe acute pancreatitis: Case report on three family members. Pancreatology 2020;20(4):665–7. [CrossRef]
[Pubmed]

4.
Aloysius MM, Thatti A, Gupta A, Sharma N, Bansal P, Goyal H. COVID-19 presenting as acute pancreatitis. Pancreatology 2020;20(5):1026–7. [CrossRef]
[Pubmed]

5.
Parenti DM, Steinberg W, Kang P. Infectious causes of acute pancreatitis. Pancreas 1996;13(4):356–71. [CrossRef]
[Pubmed]

6.
Liu F, Long X, Zhang B, Zhang W, Chen X, Zhang Z. ACE2 expression in pancreas may cause pancreatic damage after SARS-CoV-2 infection. Clin Gastroenterol Hepatol 2020;18(9):2128–30.e2. [CrossRef]
[Pubmed]

7.
Ferm S, Fisher C, Pakala T, et al. Analysis of gastrointestinal and hepatic manifestations of SARS-CoV-2 infection in 892 patients in queens, NY. Clin Gastroenterol Hepatol 2020;18(10):2378–9.e1. [CrossRef]
[Pubmed]

SUPPORTING INFORMATION
Author Contributions
Manoj Kolhe - Conception of the work, Design of the work, Acquisition of data, Drafting the work, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Praveen Sharma - Conception of the work, Design of the work, Acquisition of data, Analysis of data, Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Shrihari Anikhindi - Acquisition of data, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Naresh Bansal - Acquisition of data, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Munish Saachdeva - Acquisition of data, Drafting the work, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Anil Arora - Acquisition of data, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Guarantor of SubmissionThe corresponding author is the guarantor of submission.
Source of SupportNone
Consent StatementWritten informed consent was obtained from the patient for publication of this article.
Data AvailabilityAll relevant data are within the paper and its Supporting Information files.
Conflict of InterestAuthors declare no conflict of interest.
Copyright© 2020 Manoj Kolhe et al. This article is distributed under the terms of Creative Commons Attribution License which permits unrestricted use, distribution and reproduction in any medium provided the original author(s) and original publisher are properly credited. Please see the copyright policy on the journal website for more information.