|
Research Article
Quality of life after repair of iatrogenic bile duct injury of postcholecystectomy Filipino patients
1 Chairman, Department of Surgery, University of the Philippines College of Medicine and Philippine General Hospital, Philippines
2 Surgical Resident, Manila Doctors Hospital, Philippines
3 Associate Professor, Department of Surgery, University of the Philippines College of Medicine and Philippine General Hospital, Philippines
Address correspondence to:
Anthony R Perez
Associate Professor, Department of Surgery, University of the Philippines College of Medicine and Philippine General Hospital,
Philippines
Message to Corresponding Author
Article ID: 100086Z04CA2020
Access full text article on other devices

Access PDF of article on other devices

How to cite this article
Arcilla CE, Zamora HPA, Perez AR. Quality of life after repair of iatrogenic bile duct injury of postcholecystectomy Filipino patients. Int J Hepatobiliary Pancreat Dis 2020;10:100086Z04CA2020.ABSTRACT
Aims: The estimated incidence of bile duct injuries (BDIs) has increased ranging from 0.4% to 0.7% since global recognition of laparoscopic cholecystectomy as a standard procedure. Bile duct injuries are associated with increased morbidity and mortality, as well as substantial health care costs, and malpractice litigation claims. This study aims to determine the quality of life (QoL) of Filipino patients after repair of BDIs incurred from their previous laparoscopic or open cholecystectomies.
Methods: A total of 22 patients post-repair of BDIs and 22 age- and sex-matched patients who had unremarkable cholecystectomies from 1997 to 2017 were recruited for this study. The patients were requested to answer a survey on QoL using RAND 36-Item Health Survey 1.0, a validated survey which includes a multi-item scale that assesses eight health concepts.
Results: Patients with BDIs had lower scores in all domains compared to non-BDI group. Physical functioning and role limitations due to physical health are statistically significant (p values 0.0473 and 0.0025). Conclusion: The effect of BDI is considerable and bears an impact on a patient’s health and well-being. Physical functioning and role limitations due to physical health were identified to be impaired among these patients and these factors should be assessed during long-term follow-up.
Keywords: Bile duct injury, Bile duct reconstruction, Quality of life
Introduction
Laparoscopic cholecystectomy has been the standard of care for the treatment of gallstone diseases. This technique offers the patient the advantages of minimal invasive surgery, such as better cosmetic result, faster postoperative recovery, and shorter hospital stay [1]. Although laparoscopic cholecystectomy is the gold standard for symptomatic cholecystitis, surgeons still use the open method in 10–30% of cases [1] [2].
However with the widespread acceptance of this operation all over the world, the spectrum of complications in gallstone surgery has changed [3], resulting to an increased frequency of biliary duct injuries [4].
The estimated incidence of major BDIs during the open cholecystectomy era was 0.1–0.3%, but has risen to an estimated 0.4–0.6% after the introduction of laparoscopic cholecystectomy [4]. Several published studies have reported similar rates, ranging from 0.4% to 0.7% [4],[5]. Bile duct injuries are associated with increased morbidity and mortality, as well as substantial health care costs [6] and malpractice litigation claims. Bile duct injury likewise leads to long-term mortality, particularly those requiring operative intervention [7]. Although long-term studies have shown diminished survival of patients sustaining bile leaks major duct injuries, better outcomes are seen in those undergoing surgical repair compared to endoscopic intervention alone [8].
Independent studies of de Reuver et al. (2009) and Moore et al. (2004) on 278 and 86 patients with BDI injuries postlaparoscopic cholecystectomy showed long-term detrimental effects on health-related QoL and do not improve on follow-up [9],[10]. Mental health concerns were more commonplace compared to physical or general health concerns at the time of BDIs, with patients reporting a depressed mood or low energy level [11].
Other studies reported different results. Two separate case control studies done by Karvonen et al. (2013) on 51 BDI patients and Hogan et al. (2009) on 62 patients showed that there were no major differences in QoL between patients with BDIs and patients who underwent an uneventful laparoscopic cholecystectomy with a mean follow-up of 8 years and 12 years, respectively [12],[13].
Quality of life improves significantly after the first year of surgical repair, reaching a plateau at five years [14]. With a minimum of five years of follow-up, the QoL after surgical biliary reconstruction compares favorably with that of patients undergoing uneventful cholecystectomy [15].
Currently, our local data is limited and incidence of BDIs has yet to be defined. Quality of life among Filipino patients who have had BDIs sustained during laparoscopic or open cholecystectomies has yet to be determined. This study is a cross-sectional study which aims to evaluate the QoL of Filipino patients with BDIs associated with laparoscopic or open cholecystectomies to help clinicians better understand these patients and address any health concerns to improve their well-being.
MATERIALS AND METHODS
Study design
The study protocol was reviewed and approved by the Manila Doctors Hospital Institutional Review Board. This study is a cross-sectional study, aimed to determine the status of the QoL of Filipino patients after repair of BDIs after laparoscopic or open cholecystectomy as compared with patients with unremarkable postlaparoscopic or open cholecystectomy postoperative course.
Subjects
Sample size is computed using Stata SE Version 13. The minimum sample size requirement is 42 participants for the total population (BDI and non-BDI patients) based on the SF-36 scores of patients with and without BDI (Boerma et al., 2001) with significance level 5% and power of 90%.
A total of 44 participants were gathered for the study. Patients with gallbladder stone disease who underwent laparoscopic or open cholecystectomies were included. Patients with other gallbladder diseases and biliary diseases, such as malignancy, were excluded from the study. The first group included 22 patients who sustained bile-duct injuries during laparoscopic or open cholecystectomy and had eventually undergone repair of the injury. Only patients who sustained injuries requiring reconstruction with a hepaticojejunostomy were included in the study. All patients sustained their injuries from surgeries performed in other hospitals and were referred to the reporting institution ready for reconstruction. Patients who were managed definitively with endoscopic or with percutaneous techniques were not included. The second group included 22 patients with unremarkable postlaparoscopic or open cholecystectomies, age-and gender-matched to the case subjects. All reconstructive biliary repair surgeries and uneventful cholecystectomy surgeries of these patients were done by a single biliary specialist surgeon (CA).
Quality of life outcome tool used is the RAND 36-Item Health Survey 1.0. This is a self-administered validated questionnaire which includes a multi-item scale that assesses eight health concepts: (1) limitations in physical activities because of health problems; (2) limitations in social activities because of physical or emotional problems; (3) limitations in usual role activities because of physical health problems; (4) bodily pain; (5) general mental health (psychological distress and well-being); (6) limitations in usual role activities because of emotional problems; (7) vitality (energy and fatigue); and (8) general health perceptions [16],[17]. English and Filipino versions of the RAND 36 questionnaire were both given to all participants for this study [18].
Procedure
Participants were identified through chart review and nonrandomly selected from personal log of the main author. Participants were selected based on the inclusion–exclusion criteria stated above. A written informed consent explaining the research study was taken from the patients. Patients who gave their consent were asked to answer both the English and Filipino versions of the RAND 36 questionnaire. Individual scores were collated for interpretation based on the RAND 36 scoring algorithm [16]. Quality of life scores were derived in the following manner: Step 1 entails the transcribing of the original responses into numeric values as stated in the scoring protocol of the RAND 36 version 1.0. Step 2 entails the summation and averaging of items within scales to derive the eight (8) scale scores [17]. Scores of both groups were compared using T-tests and Fisher test.
RESULTS
Study population
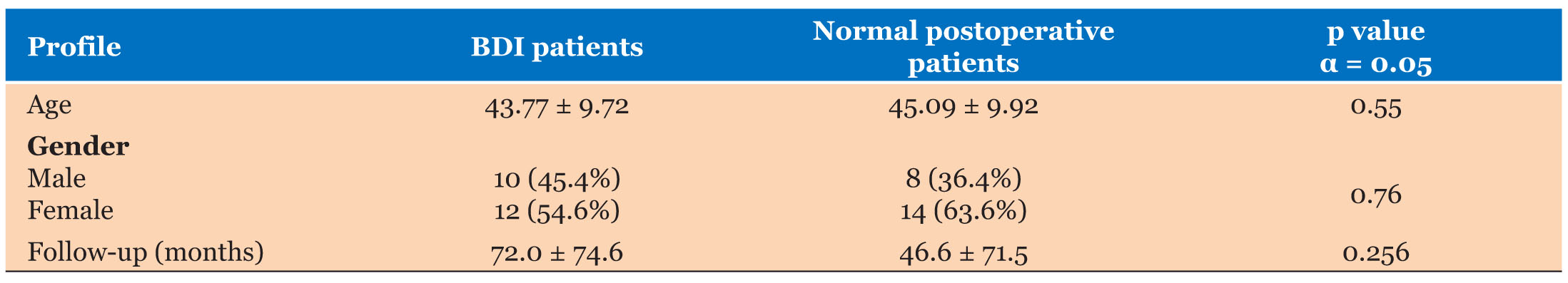
A total of 44 patients were recruited for this study and all RAND-36 surveys were returned and answered completely, with 100% response rate from both groups. Study groups were similar with respect to age, gender, and follow-up time from initial surgery to completion of the RAND-36 questionnaire (see Table 1). All patients were interviewed more than a year after their last surgical intervention.
T-tests and Fisher test revealed no significant differences between the two groups, with regard to age, gender, and time of follow-up (p values 0.55, 0.76, and 0.256, respectively).
Assessment of quality of life (QoL)
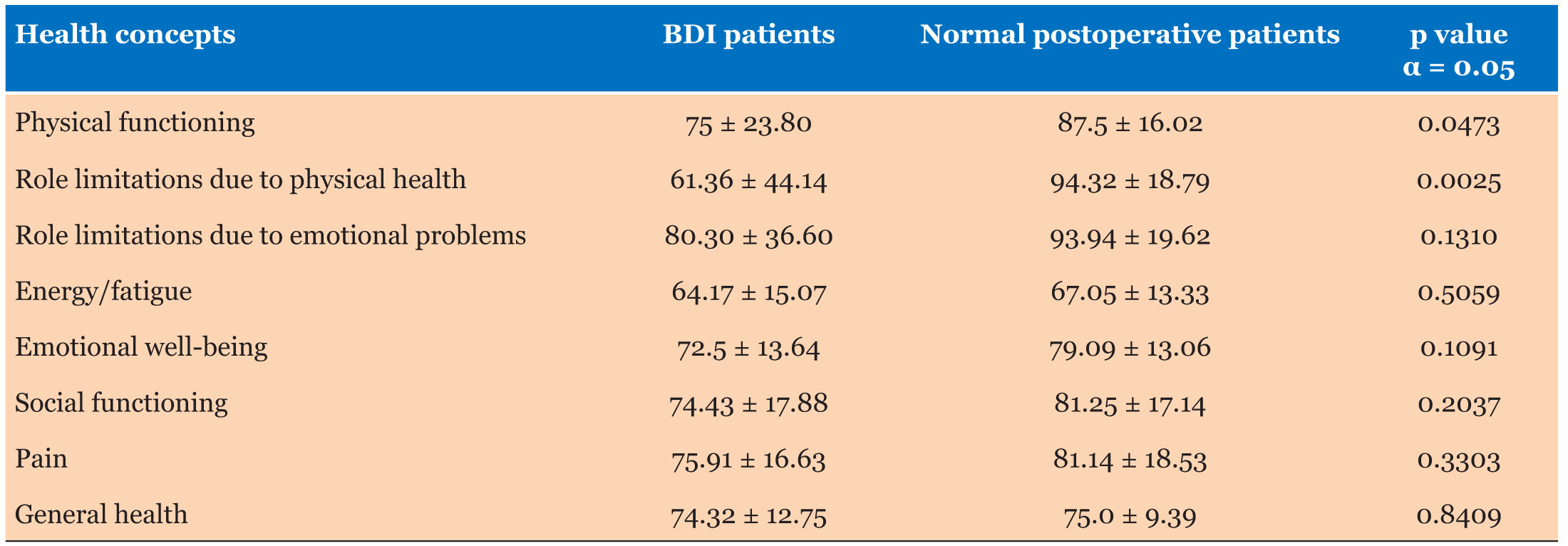
Overall QoL scores for BDI patients and uncomplicated postcholecystectomy patients are shown in Table 2. Patients with BDIs had lower scores in all domains as compared to patients with unremarkable postcholecystectomies. Among the health concepts in the survey, physical functioning and role limitations due to physical health are significantly different between the two groups, with the BDI group scoring lower than the control group.
Other health concepts such as role limitations due to emotional problems, energy and fatigue, emotional well-being, social functioning, pain, and general health were not statistically significant between the two groups.
Discussion
Our results showed generally lower QoL scores with BDI patients as compared to patients with unremarkable postoperative course. These patients have impaired QoL in terms of physical functions, such as basic self-care activities, such as bathing, or dressing, as well as work-related activities, such as housework and career.
The physical limitations of these Filipino patients identified in this study may have been brought about by their BDIs incurred during their first operation, the need for subsequent operations for biliary repair and reconstruction, and the prolonged period of recovery to be endured every after a procedure or surgery is done. Physical activities of these patients are restricted to a certain degree, with some requiring assistance to carry out daily tasks.
Interestingly, these Filipino BDI patients compare favorably with healthy controls in terms of mental health, social functions, vitality, and general health perceptions. These scores may likely be due to strong family ties and stable support group observed among Filipino patients, giving them a good outlook in life and still enabling them to socialize with others.
This study focused mainly on BDI Filipino patients, a subset of patients who have received less attention in terms of local study and research mainly due to the difficulty in gathering a larger sample size. Cases on BDIs are sensitive, and a meticulous documentation and communication with these patients are crucial to achieve a successful study.
Our results showed significantly low scores for physical functioning of BDI patients during their recovery. Physical assistance in these patients’ daily routine must be emphasized and instructed to family members by their respective physicians.
As of the time of writing, this is the only local study which dealt on BDI Filipino patients. This study will enable physicians and surgeons in the country to better understand this subset of Filipino patients in terms of their general health, thus allowing holistic approach to postoperative care.
Conclusion
The effect of BDI is considerable and bears an impact on a patient’s health and well-being. We report the first study to examine the health-related QoL outcomes among Filipino patients who have sustained BDIs during cholecystectomies. Physical functioning and role limitations due to physical health were identified to be impaired among these patients. These factors should be assessed during follow-up and monitored closely.
LIMITATIONS OF THE STUDY
Study limitations include a small sample size. This was expected considering that this is a single institution study collecting an event with low incidence. A largescale multicenter study is recommended to achieve better representation of Filipino BDI patients. Likewise, combining and analyzing patients who sustained BDIs from both open and laparoscopic cholecystectomies may have rendered the group heterogenous. A subgroup analysis would have been more informative but the smaller sample size may further diminish the power of our results. We were hoping that obtaining the scores more than a year for all the patients would have already negated the differences in QoL attributable to the type of incision. Further studies on this matter will have to address these limitations.
REFERENCES
1.
Boerma D, Rauws E, Keulemans YC, et al. Impaired quality of life 5 years after bile duct injury during laparoscopic cholecystectomy: A prospective analysis. Ann Surg 2001;234(6):750–7. [CrossRef]
[Pubmed]

2.
Wolf AS, Nijsse BA, Sokal SM, Chang Y, Berger DL. Surgical outcomes of open cholecystectomy in the laparoscopic era. Am J Surg 2009;197(6):781–4. [CrossRef]
[Pubmed]

3.
Shamiyeh A, Wayand W. Laparoscopic cholecystectomy: Early and late complications and their treatment. Langenbecks Arch Surg 2004;389(3):164–71. [CrossRef]
[Pubmed]

4.
Melton GB, Lillemoe KD, Cameron JL, Sautes PA, Coleman J, Yeo CJ. Major bile duct injuries associated with laparoscopic cholecystectomy: Effect of surgical repair on quality of life. Ann Surg 2002;235(6):888–95. [CrossRef]
[Pubmed]

5.
Landman MP, Feurer ID, Moore DE, Zaydfudin V, Pinson CW. The long-term effect of bile duct injuries on health-related quality of life: A meta-analysis. HPB (Oxford) 2013;15(4):252–9. [CrossRef]
[Pubmed]

6.
Savader SJ, Lillemoe KD, Prescott CA, et al. Laparoscopic cholecystectomy-related bile duct injuries: A health and financial disaster. Ann Surg 1997;225(3):268–73. [CrossRef]
[Pubmed]

7.
Halbert C, Altieri MS, Yang J, et al. Long-term outcomes of patients with common bile duct injury following laparoscopic cholecystectomy. Surg Endosc 2016;30(10):4294–9. [CrossRef]
[Pubmed]

8.
Fong ZV, Pitt HA, Strasberg SM, et al. Diminished survival in patients with bile leak and ductal injury: Management strategy and outcomes. J Am Coll Surg 2018;226(4):568–76.e1. [CrossRef]
[Pubmed]

9.
de Reuver PR, Sprangers MA, Rauws EA, et al. Impact of bile duct injury after laparoscopic cholecystectomy on quality of life: A longitudinal study after multidisciplinary treatment. Endoscopy 2008;40(8):637–43. [CrossRef]
[Pubmed]

10.
Moore DE, Feurer ID, Holzman MD, et al. Long-term detrimental effect of bile duct injury on health-related quality of life. Arch Surg 2004;139(5):476–81. [CrossRef]
[Pubmed]

11.
Ejaz A, Spolverato G, Kim Y, Dodson R, et al. Long-term health-related quality of life after iatrogenic bile duct injury repair. J Am Coll Surg 2014;219(5):923-32.e10. [CrossRef]
[Pubmed]

12.
Karvonen J, Grönroos JM, Mäkitalo L, Koivisto M, Salminen P. Quality of life after iatrogenic bile duct injury – A case control study. Minim Invasive Ther Allied Technol 2013;22(3):177–80. [CrossRef]
[Pubmed]

13.
Hogan AM, Hoti E, Winter DC, et al. Quality of life after iatrogenic bile duct injury: A case control study. Ann Surg 2009;249(2):292–5. [CrossRef]
[Pubmed]

14.
Dominguez-Rosado I, Mercado MA, Kauffman C, Ramirez-del Val F, Elnecavé-Olaiz A, Zamora-Valdés D. Quality of life in bile duct injury: 1-, 5-, and 10-year outcomes after surgical repair. J Gastrointest Surg 2014;18(12):2089–94. [CrossRef]
[Pubmed]

15.
Sarmiento JM, Farnell MB, Nagorney DM, Hodge DO, Harrington JR. Quality-of-life assessment of surgical reconstruction after laparoscopic cholecystectomy-induced bile duct injuries: What happens at 5 years and beyond? Arch Surg 2004;139(5):483–8. [CrossRef]
[Pubmed]

16.
Ware JE Jr, Sherbourne CD. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care 1992;30(6):473–83.
[Pubmed]

17.
Hays RD, Sherbourne CD, Mazel RM. The RAND 36-item health survey 1.0. Health Econ 1993;2(3):217–27. [CrossRef]
[Pubmed]

18.
Bataclan RP, Dial MA. Cultural adaptation and validation of the filipino version of kidney disease quality of life – short form (KDQOL-SF version 1.3). Nephrology (Carlton) 2009;14(7):663–8. [CrossRef]
[Pubmed]

SUPPORTING INFORMATION
Author Contributions
Crisostomo E Arcilla - Conception of the work, Design of the work, Acquisition of data, Analysis of data, Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Hector Paolo A Zamora - Conception of the work, Design of the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Anthony R Perez - Conception of the work, Design of the work, Drafting the work, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Guarantor of SubmissionThe corresponding author is the guarantor of submission.
Source of SupportNone
Consent StatementWritten informed consent was obtained from the patient for publication of this article.
Data AvailabilityAll relevant data are within the paper and its Supporting Information files.
Conflict of InterestAuthors declare no conflict of interest.
Copyright© 2020 Crisostomo E Arcilla et al. This article is distributed under the terms of Creative Commons Attribution License which permits unrestricted use, distribution and reproduction in any medium provided the original author(s) and original publisher are properly credited. Please see the copyright policy on the journal website for more information.