|
Research Article
Platelet transfusion practices in neonatology: A single-center observational study
1 Pediatric Hematology-Oncology Fellow, Department of Pediatrics, Division of Pediatric Hematology-Oncology, Montreal Children’s Hospital, McGill University, Montreal, Québec, Canada
2 Pediatric Intensivist, Department of Pediatrics, Division of Pediatric Intensive Care, CHU Sainte-Justine, Université de Montréal, Montreal, Québec, Canada
3 Neonatologist, Department of Pediatrics, Division of Neonatology, CHU Sainte-Justine, Université de Montréal, Montreal, Québec, Canada
4 Emergency Physician, Department of Emergency Medicine, Hôpital du Sacré-Coeur de Montréal, Université de Montréal, Montreal, Québec, Canada
Address correspondence to:
Alexandra Zabeida
313 rue Caisse, Verdun, QC H4G 3M3,
Canada
Message to Corresponding Author
Article ID: 100072Z02AZ2022
Access full text article on other devices

Access PDF of article on other devices

How to cite this article
Zabeida A, Lacroix J, Lapointe A, Lachance C, Cournoyer A, Villeneuve A. Platelet transfusion practices in neonatology: A single-center observational study. Int J Blood Transfus Immunohematol 2022;12:100072Z02AZ2022.ABSTRACT
Aims: Platelet transfusions are common in the neonatal intensive care unit (NICU), yet practices vary substantially. This study aims to determine platelet transfusion incidence, determinants, and justifications in neonatology.
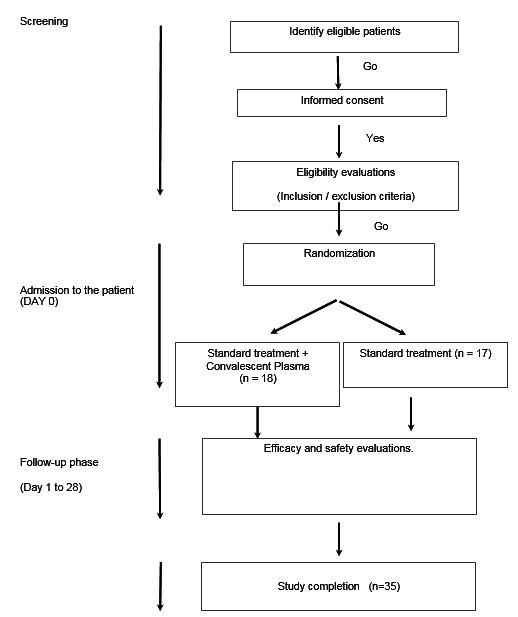
Methods: Single-center prospective cohort study, including all patients consecutively admitted to the CHU Sainte-Justine Hospital NICU over a 5-month period in 2013. Data were collected by chart review and transfusion justifications were assessed using a questionnaire.
Results: A total of 401 participants were included. Mean birth weight (BW) was 2.34±1.01 kg and gestational age (GA) was 34.4±4.5 weeks. Thirty-seven neonates (9.2%) received at least one platelet transfusion. Platelet-transfused neonates were mostly extremely preterm (40.5%) or term (24.3%). The median pre-platelet transfusion count was 57 × 109/L (9–285 × 109/L). Compared to non-transfused patients, those who received at least one platelet transfusion had a significantly lower BW and GA, higher CRIB-II and SNAPPE-II scores (all p <0.001) and were more frequently admitted for respiratory disease (p <0.001), hypoxic-ischemic encephalopathy (p=0.009), and hemolytic disease of the newborn (p <0.001). Gestational age <28 weeks (p<0.001), mechanical ventilation requirements (p=0.008), and platelet nadir ≤150 × 109/L (p<0.001) upon admission were independently associated with a higher risk of platelet transfusion in this cohort. Most frequent justifications for ordering a first platelet transfusion were low platelet counts (86.5%), underlying disease (78.4%) and illness severity (37.8%).
Conclusion: Pre-transfusion platelet counts in neonates varied widely and were higher than the thresholds proposed in the literature. Several factors other than platelet count predicted risk of platelet transfusion in this cohort.
Keywords: Neonatology, Platelet, Thrombocytopenia, Transfusion
SUPPORTING INFORMATION
Acknowledgments
We would like to thank Miguel Chagnon for his contribution to the statistical analysis, as well as the Fonds Fonds de la Recherche du Québec—Santé for funding this project.
Author ContributionsAlexandra Zabeida - Acquisition of data, Analysis of data, Interpretation of data, Drafting the article, Revising it critically for important intellectual content, Final approval of the version to be published
Jacques Lacroix - Substantial contributions to conception and design, Revising it critically for important intellectual content, Final approval of the version to be published
Anie Lapointe - Substantial contributions to conception and design, Acquisition of data, Analysis of data, Interpretation of data, Drafting the article, Revising it critically for important intellectual content, Final approval of the version to be published
Christian Lachance - Revising it critically for important intellectual content, Final approval of the version to be published
Alexis Cournoyer - Revising it critically for important intellectual content, Final approval of the version to be published
Andréanne Villeneuve - Substantial contributions to conception and design, Acquisition of data, Analysis of data, Interpretation of data, Revising it critically for important intellectual content, Final approval of the version to be published
Guarantor of SubmissionThe corresponding author is the guarantor of submission.
Source of SupportNone
Consent StatementWritten informed consent was obtained from the patient for publication of this article.
Data AvailabilityAll relevant data are within the paper and its Supporting Information files.
Conflict of InterestAuthors declare no conflict of interest.
Copyright© 2022 Alexandra Zabeida et al. This article is distributed under the terms of Creative Commons Attribution License which permits unrestricted use, distribution and reproduction in any medium provided the original author(s) and original publisher are properly credited. Please see the copyright policy on the journal website for more information.