 |
Research Article
Multicenter retrospective cohort study: Using trends in liver function tests to predict spontaneous passage of common bile duct stones in choledocholithiasis
1 General Surgery Registrar, Associate Lecturer, University of Queensland Surgical Division, Redcliffe Hospital Metro North Health, Anzac Ave, Redcliffe, QLD 4020, Australia
2 General Surgery Registrar, Surgical Division, Mackay Base Hospital, 475 Bridge Road, Mackay, QLD 4740, Australia
3 Urology Department, Palmerston North Hospital, 50 Ruahine Street, Roslyn, Palmerston North 4442, New Zealand
4 General Surgery Consultant, Surgical Division, Redcliffe Hospital Metro North Health, Anzac Ave, Redcliffe, QLD 4020, Australia
Address correspondence to:
Bardia Bidarmaghz
Redcliffe Hospital, Anzac Avenue, Redcliffe, QLD 4053,
Australia
Message to Corresponding Author
Article ID: 100102Z04BB2023
Access full text article on other devices

Access PDF of article on other devices

How to cite this article
Bidarmaghz B, Sabat N, Sharma A, McGregor H, Wong J. Multicenter retrospective cohort study: Using trends in liver function tests to predict spontaneous passage of common bile duct stones in choledocholithiasis. Int J Hepatobiliary Pancreat Dis 2023;13(1):7–14.ABSTRACT
Aim: Endoscopic retrograde cholangiopancreatography (ERCP) is the modality of choice in patients who are diagnosed with choledocholithiasis, but it carries potentially life-threatening risks and is not readily available in rural hospitals. Due to the lack of access to this service, trend of liver function tests is often used to predict the spontaneous passage of common bile duct (CBD) stone to prevent performing a negative ERCP. The aim of this study is to investigate whether the trend of liver function tests can be used to predict passage of common bile duct stone in patients who have radiological evidence of choledocholithiasis.
Methods: The liver function tests (LFTs) of patients diagnosed with choledocholithiasis at two separate hospitals in New Zealand and Australia were collected at two points retrospectively. The change in LFT values between diagnosis and immediately prior to ERCP was analyzed.
Results: Total of 409 patients were selected with 108 (26%) and 301 (74%) patients from Australia and New Zealand, respectively. Demographic and LFT values were statistically different between the two centers, but the female sex was significantly predominant in both. Cumulative data showed that 37% of patients diagnosed with choledocholithiasis had no stone during the ERCP procedure. Increased age was statistically significant in patients with a persistent stone on ERCP. Importantly, there was no statistical difference between LFT values of patients with persistent gallstones shown on ERCP compared to those who have passed their gallstones spontaneously. Aspartate aminotransferase (AST) was significantly associated with a persistent gallstone (p = 0.041), but its clinical value is questionable.
Conclusion: Decreasing trend in LFTs and their individual components are poor predictors of persistent gallstones in patients diagnosed with choledocholithiasis. Two-thirds of these patients have persistent stones and ERCP remains an important diagnostic and therapeutic modality for patients at significant risk of disease complications.
Keywords: Cholangiopancreatography, Cholangitis, Choledocholithiasis, ERCP, Liver function test, Magnetic resonance
Introduction
Gallstones or cholelithiasis is common in the western population with literature suggesting a 6% incidence in men and 9% incidence in women [1] in comparison to Asian population with the prevalence of 3–15% and nearly non-existent (less than 5%) in Africans [2]. Although the incidence increases with age, female patients are still affected more than male patients at a 2 to 1 ratio [1],[3] and many recent studies have shown that it is related to age, metabolic disorders, such as obesity, dyslipidemia, and type 2 diabetes [4]. The vast majority of these individuals have asymptomatic or incidentally found gallstones which will remain asymptomatic for life [3]. The spectrum of symptomatic gallstone disease ranges from biliary colic and cholecystitis, reflecting gallstone impaction within the gallbladder or cystic duct causing obstruction, to choledocholithiasis with or without acute cholangitis and gallstone pancreatitis, which reflect gallstone obstruction of the common bile duct [5]. These common bile duct stones result from either migration of a gallstone from the gallbladder or de novo formation of gallstones within the duct by intraductal precipitation due to bile stasis within a biliary diverticulum or a large bile duct [6]. This article looked at the subset of patients who have choledocholithiasis where the diagnosis and treatment of these gallstones remain controversial.
Choledocholithiasis is found in 10% of patients presenting with symptomatic gallstone disease [7]. This figure increases to 15% of patients if you look at patients specifically presenting with acute cholecystitis [7]. Choledocholithiasis is suspected based on the clinical history and physical examination but the diagnosis is made based on a combination of laboratory tests and radiological investigations [5]. Liver function tests (LFTs) typically show a cholestatic pattern with a disproportionate elevation in bilirubin, alkaline phosphatase, and gamma-glutamyl transferase (GGT) [8]. However, many studies have attempted and failed to validate specific investigations, including LFTs, to diagnose the presence of persistent gallstones in the common bile duct without further imaging on presentation [8]. Additionally, studies have shown individual components of the LFTs have poor predictive for the presence of choledocholithiasis on presentation [8]. Alongside the laboratory tests, the radiological study of choice for patients suspected of having choledocholithiasis is a targeted abdominal ultrasound [9]. Magnetic resonance cholangiopancreatography (MRCP) is an additional test better able to characterize the biliary tract and identify gallstones within the distal common bile duct, especially in a patient with previous gastrointestinal tract surgeries [9],[10].
After the diagnosis of choledocholithiasis, a patient may undergo a therapeutic endoscopic retrograde cholangiopancreatography (ERCP), cholecystectomy with intraoperative common bile duct exploration, or a cholecystectomy with subsequent interval ERCP. To date, ERCP remains the gold standard test for diagnosis and definitive treatment of choledocholithiasis [11]. However, ERCP carries significant risks including 15% risk of postoperative pancreatitis, a 1–2% risk of post-endoscopic sphincterotomy bleeding, upper intestinal perforation, and postoperative infection [12],[13].
Study rationale
Endoscopic retrograde cholangiopancreatography relies on the availability of skilled clinicians who are often not available in regional and rural hospitals around Australia. Additionally, endoscopists considering a therapeutic ERCP for the treatment of choledocholithiasis often rely on the trends in LFTs to determine which patients would most benefit from this procedure. In rural and regional centers in Australia where access to ERCP is limited, monitoring LFTs can become a barrier for the patients with choledocholithiasis to have access to ERCP in a timely manner. Therefore, this study will look at the basis of this decision process to evaluate the validity of using LFTs in patient selection for ERCPs. Alternatively, patients may need to be transferred to large tertiary centers. This interval ERCP, whether days or months, may be preceded by spontaneous passage of gallstones leading to a negative ERCP in patients with previously diagnosed choledocholithiasis [6],[8]. This study additionally investigates the value of laboratory investigations in this niche situation to help eliminate the risks of a potentially unnecessary procedure, reducing procedure related complications, hospital waitlist burdens, and improving waitlist times.
Liver function tests, well known to show a cholestatic picture in choledocholithiasis, are an inexpensive investigation often available in regional and rural centers within a reasonable time. It may be postulated that on passage or removal of the stone, the enzymes would normalize in blood, a hypothesis which has not been validated to date despite multiple individual studies [8]. Interestingly, liver function tests reflecting a cholestatic picture can reveal a spike post ERCP due to the intervention but more often reveal a steady downward trend post-successful ERCP [14]. Few studies have looked at the trend of liver function tests prior to the ERCP and its applicability for patient selection. In our study, we investigate whether a downward trend in the liver function tests of a subset of patients can be used as a predictive value for spontaneous passage of the gallstone. These patients are admitted and have radiological [ultrasound, computed tomography scan, magnetic resonance cholangiopancreatography (MRCP), or intraoperative cholangiogram] evidence of choledocholithiasis and pending ERCP for the extraction of the gallstone.
MATERIALS AND METHODS
Ethics
Ethical approval was gained on 4th of September 2017 from the Human Research Ethics Committee Metro North HREC/17/QPCH/315.
Patient selection
This was a multicenter retrospective cohort study conducted in New Zealand hospital (January 2012–June 2015) and an Australian hospital (January 2014–May 2018). During these periods adult patients (age >18 years) eligible for inclusion were those who had undergone an ERCP procedure for choledocholithiasis diagnosed radiologically by ultrasound, computed tomography scan, MRCP, or intraoperative cholangiography. Another important inclusion criteria for these patients required liver function tests to be taken at two different times: initial LFT at the time of radiological diagnosis and second LFT completed within 24 hours of the patient’s ERCP procedure. Finally, the maximum time interval from radiological diagnosis of choledocholithiasis to the ERCP procedure was required to be no more than 60 days. Patients who were diagnosed with cholangitis, pancreatitis, sclerosing cholangitis, liver fibrosis, primary biliary cirrhosis, biliary tree malignancy, and patients who had undergone prior ERCP or biliary instrumentation for complicated gallstone disease or other diagnoses were excluded.
Data collection
The medical records of eligible patients within each center were reviewed retrospectively for study variables including patient age, gender, procedure location, serum liver function tests (both centers use similar values), radiological reports diagnosing choledocholithiasis, and ERCP procedure reports. Liver function tests included bilirubin total (normal range 4–24 µmol/L), alanine aminotransferase (ALT; normal range <45 U/L), aspartate aminotransferase (AST; normal range <35 U/L), alkaline phosphatase (ALP; normal range 30–110 U/L), gamma glutaryl transferase (GGT; normal range < 55 U/L). Each patient’s results were recorded at two different time points: first during radiological diagnosis of choledocholithiasis and second within 24 hours prior to ERCP procedure. The radiological reports were reviewed to confirm the diagnosis of choledocholithiasis as reported by the radiologist. ERCP procedure reports were reviewed to identify the presence or absence of a gallstone in the common bile duct during each patient’s procedure.
Outcome measures
The primary outcome measured in this study was the relationship between decreasing LFT values and the presence or absence of a gallstone on ERCP. The study participants and their collected data were separated into two distinct groups, one group where a gallstone was found on their ERCP procedure and another where no gallstone was found. Secondary variables explored include individual components of the LFT panel to explore relationship between individual LFT parameters’ trends and their ability to predict patients with and without common bile duct stones. Liver function test measurements were categorized as normal or abnormal based on the following cut offs: abnormal bilirubin >24, abnormal ALT >45, abnormal AST >35, abnormal ALP > 110, abnormal GGT >55.
Statistical analysis
Statistical analysis was completed by specialist statisticians at the QIMR Berghoffer Medical Research Institute in Queensland, Australia to ensure accurate and reliable data analysis outcomes. Patient selection data for each group was summarized using absolute frequency and percentage figures. Demographic data were summarized with mean and standard deviation for normally distributed continuous variables while categorical variables were expressed as frequency and percentage figures. To establish demographic differences between the two groups, student’s t-test was performed on normally distributed continuous variables while the chi-squared test was used for categorical variables. To determine significant difference in the two ERCP groups comparing the persistence of stones univariate analyses were performed. Liver function tests with non-normally distributed continuous variables were presented with median and interquartile range. To determine the difference in these values of the two groups a Mann–Whitney test was conducted on these non-normally distributed continuous variables. To compare the results between the two centers, univariate analyses were performed comparing the Australian and New Zealand patient data. Finally, logistic regression was used to test the hypothesis that a change in LFT values is predictive of the presence or absence of a gallstone in the ERCP procedure. Initially, univariate models were explored looking at the association between initial LFT, pre-procedure LFT and difference in LFT levels individually. Normalizing LFT differences by time, as well as modeling change as a categorical factor was considered. Given these analyses did not affect the results, these models are not presented. Multivariable models were then considered, including adjustments for age and cohort country. All analyses were carried out in R statistical computing language and environment version 3.5.0.
RESULTS
Patient selection
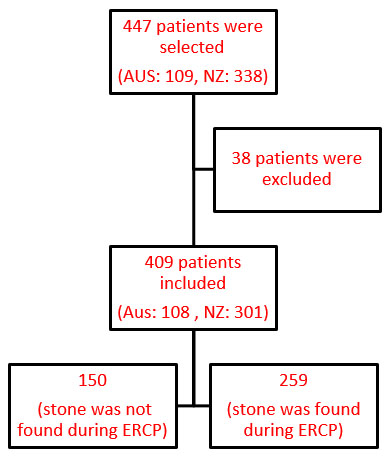
The study included 409 patients in the final analysis from a selection of 447 eligible patients, 38 were excluded due to the extended period between the diagnosis of choledocholithiasis and the ERCP procedure as shown in Figure 1.
Table 1 presents the descriptive statistics for all the patients included in the study. The statistics are also provided for the “stone found” and “no stone found” group during ERCP. Endoscopic retrograde cholangiopancreatography data showed 37% of patients diagnosed with choledocholithiasis had no gallstone found during the procedure. Patients having a persistent stone on ERCP were statistically older (65 vs 57, p = <0.001). There was a statistical difference between patients with and without a persistent gallstone in initial bilirubin (39 vs 24, p = <0.001), initial GGT (398 vs 295, p = 0.015), pre-procedure bilirubin (21 vs 14, p = < 0.001), pre-procedure ALT (110 vs 74, p = 0.009), pre-procedure AST (63 vs 44, p = 0.011), pre-procedure ALP (198 vs 159, p = 0.002), and pre-procedure GGT (344 vs 225, p = <0.001). Importantly, there was a significant difference between the two groups of patients on the LFT values completed immediately pre-procedure. Finally, the difference between the LFT values of patients with persistent gallstones shown on ERCP were not statistically different from those who have passed their gallstones spontaneously.
In Table 2, the data are broken down into Australia and New Zealand population and statistics are compared between these two countries. It shows that 108 (26%) patients were from Australia and 301 (74%) patients were from the New Zealand center. The difference in patient gender between the two centers was significant (26.9% vs 42.2%, p = 0.005), but no statistical difference in age (59.44 vs 63.03, p = 0.11). Additionally, there was a significant difference between the two centers in the initial GGT (233 vs 403, p =0.001), initial AST (165 vs 128, p = 0.02), pre-procedure bilirubin (21.5 vs 16, p = 0.027), pre-procedure ALT (165 vs 79, p =0.001), pre-procedure AST (79 vs 50, p =0.001), and difference in bilirubin (-4 vs -11, p = 0.009), GGT (-7 vs -51, p = 0.003).
The univariate logistic model adjusted for pre-procedure LFT status, and model adjusted for country and age are presented in Table 3 for each LFT outcome. The change in LFT differences were also categorized into decrease and increase/stay the same. This avoided the influence of outliers on the model. Interestingly a decrease in AST was associated with having a stone; however, the biologically plausibility must be taken into consideration. The odds ratio for the univariate model indicates that if a subject has a decrease in AST, they have 60% increased odds of having a stone. This effect remained after adjusting for whether AST was abnormal at pre-procedure, age, and country.
Multiple logistic regression analysis showed a decrease in AST as significantly associated with a persistent gallstone (p = 0.041) (Table 3). This remains significant when the model is adjusted for pre-procedure LFT status (p = 0.023) and when adjusted for both country and age (p = 0.037). Otherwise, the regression analysis in Table 3 showed no other statistically significant parameter in predicting the presence of gallstones at the time of the patients’ ERCP procedure.
Discussion
Given current practices of endoscopists in rural Australian hospitals the primary aim of this study was to demonstrate that a decline in the liver function tests or one of its individual parameters can predict spontaneous passage of obstructing gallstones. Given the paucity of conclusive research in this area it was important to explore these criteria used by endoscopists to determine which patients would benefit from a therapeutic ERCP while preventing the risks of a negative ERCP. Persistent gallstones in the common bile duct can have significant morbidity and mortality from disease complications including cholangitis and pancreatitis, both potentially lethal [13]. On the other hand, the gold standard treatment for this condition is the ERCP procedure which itself has potentially life-threatening complications [12],[13]. This study aimed to explore current practices of using a cheap and accessible blood test which can be used to decrease the rate of negative or non-therapeutic ERCP procedures on patients avoiding possible complications without any benefit.
It has been established that LFTs have more than 90% sensitivity in detecting obstruction in the bile flow when ALP, GGT, and bilirubin are disproportionately increased compared to the AST and ALT which measure hepatocellular function [15],[16]. Our results show that an LFT derangement in both patient groups was consistent with this evidence. Furthermore, the bilirubin and GGT were statistically greater in the initial LFTs of the patients with persistent stones, an observation of unclear clinical significance. Interestingly, our results also demonstrated that all the individual pre-procedural LFTs in patients with a persistent gallstone are significantly higher than those who have passed the gallstone spontaneously. This observation suggests there may be a cut off above which a persistent stone can be suspected prior to the ERCP but the power of this study is insufficient to determine whether this cut-off is significant. This pre-procedural difference in LFTs between groups would suggest that when calculating the difference between each patient’s initial and pre-procedural LFTs there may be a significant difference between the two groups which can be used to predict the presence of a persistent stone. However, the calculated difference in this study shows no statistical difference between the individual LFT trend in those patients who passed the stone spontaneously and those who had a persistent stone found at their ERCP procedure. This finding is further supported by the multiple logistic regression analysis which showing no reliable predictive model using the decrease in individual LFT for identifying patients with a persistent gallstone. Aspartate aminotransferase was the only parameter of the LFTs which showed statistical significance, but its clinical utility is doubtful given the role of AST as a function of hepatocellular function. Remarkably, in 2005 Hayat et al. reported that elevated ALP is more sensitive than elevated AST in obstructing jaundice due to stricture, but in obstructive gallstone disease the rise in AST may be equal to ALP or even exceed it during maximum jaundice and painful episode [17] .
The demographic data of this study showed a significant difference between the group of patients who passed the gallstone spontaneously compared to those who had a persistent stone (57 vs 65 respectively; p =0.001). The spontaneous passage of gallstones is well recognized by Frossard et al. at a rate of 21% [18]. According to the pathophysiology of gallstone formation, the formation of stones is time dependent and increases with age [2]. Therefore, this difference in age may reflect increasing size of stone with age leading to increased difficulty in spontaneous passage of stone. This was reflected by the study of Frossard et al. which also concluded that the size of stones matters, with gallstones whose diameter is greater than 8 mm had only a 4.3% chance of spontaneous passage [18].
This study had several limitations. First, the data from each individual center were heterogenous at times with the initial comparison showing a gender disparity between the two centers. Although there is female predominance in gallstone disease, choledocholithiasis specifically has not been shown to have increased incidence in either sex [5]. As discussed in the results section, there was a significant difference LFT data of the two centers in the initial LFTs, pre-procedural LFTs, and the LFT differential. This difference between two centers showed no consistent pattern in a particular LFT parameter suggesting a possibility of type 2 statistical error. Otherwise, an important limitation is the difficulty in assessing and controlling for confounding factors in this retrospective study such as pregnancy, cholestatic medications, or confounding undiagnosed gallbladder disease listed as exclusion criteria.
Conclusion
Contrary to current practices by endoscopists in rural Australian hospitals, a decreasing trend in LFTs and its individual components are poor predictors of persistent gallstones in patients diagnosed with choledocholithiasis. This suggests the trend in LFTs is not a reliable criterion for determining patients who would most benefit from a therapeutic ERCP but may instead create an unnecessary delay in a therapeutic procedure. However, pre-procedural LFTs are significantly greater globally between the two groups and future studies may show a critical value for individual LFTs to predict persistent gallstones. Clinically given almost 2 out of every 3 patients with choledocholithiasis have persistent stones, a timely ERCP remains an important diagnostic and therapeutic modality for patients at significant risks of disease complications.
REFERENCES
1.
Everhart JE, Khare M, Hill M, Maurer KR. Prevalence and ethnic differences in gallbladder disease in the United States. Gastroenterology 1999;117(3):632–9. [CrossRef]
[Pubmed]

2.
Miquel JF, Covarrubias C, Villaroel L, et al. Genetic epidemiology of cholesterol cholelithiasis among Chilean Hispanics, Amerindians, and Maoris. Gastroenterology 1998;115(4):937–46.
[Pubmed]

3.
Diehl AK. Epidemiology and natural history of gallstone disease. Gastroenterol Clin North Am 1991;20(1):1–19. [CrossRef]
[Pubmed]

4.
Katsika D, Tuvblad C, Einarsson C, Lichtenstein P, Marschall HU. Body mass index, alcohol, tobacco and symptomatic gallstone disease: A Swedish twin study. J Intern Med 2007;262(5):581–7. [CrossRef]
[Pubmed]

5.
Tazuma S. Gallstone disease: Epidemiology, pathogenesis, and classification of biliary stones (common bile duct and intrahepatic). Best Pract Res Clin Gastroenterol 2006;20(6):1075–83. [CrossRef]
[Pubmed]

6.
Chhoda A, Jain D, Singhal S. Sex-related differences in predicting choledocholithiasis using current American Society of Gastrointestinal Endoscopy risk criteria. Ann Gastroenterol 2017;30(6):682–7. [CrossRef]
[Pubmed]

7.
Frossard JL, Morel PM. Detection and management of bile duct stones. Gastrointest Endosc 2010;72(4):808–16. [CrossRef]
[Pubmed]

8.
Panda N, Chang Y, Chokengarmwong N, et al. Gallstone pancreatitis and choledocholithiasis: Using imaging and laboratory trends to predict the likelihood of persistent stones at cholangiography. World J Surg 2018;42(10):3143–9. [CrossRef]
[Pubmed]

9.
Gurusamy KS, Giljaca V, Takwoingi Y, Higgie D, Poropat G, Štimac D, Davidson BR. Ultrasound versus liver function tests for diagnosis of common bile duct stones. Cochrane Database Syst Rev 2015;2015(2):CD011548. [CrossRef]
[Pubmed]

10.
Copelan A, Kapoor BS. Choledocholithiasis: Diagnosis and management. Tech Vasc Interv Radiol 2015;18(4):244–55. [CrossRef]
[Pubmed]

11.
Prat F, Amouyal G, Amouyal P, et al. Prospective controlled study of endoscopic ultrasonography and endoscopic retrograde cholangiography in patients with suspected common-bileduct lithiasis. Lancet 1996;347(8994):75–9. [CrossRef]
[Pubmed]

12.
Freeman ML. Complications of endoscopic sphincterotomy. Endoscopy 1998;30(9):A216–20. [CrossRef]
[Pubmed]

13.
Loperfido S, Angelini G, Benedetti G, et al. Major early complications from diagnostic and therapeutic ERCP: A prospective multicenter study. Gastrointest Endosc 1998;48(1):1–10. [CrossRef]
[Pubmed]

14.
Silverman WB, Thompson RA. Management of asymptomatically/minimally symptomatic post-ERCP serum liver test elevations: First do no harm. Dig Dis Sci 2002;47(7):1498–501. [CrossRef]
[Pubmed]

15.
Tham TC, Collins JS, Watson RG, Ellis PK, McIlrath EM. Diagnosis of common bile duct stones by intravenous cholangiography: Prediction by ultrasound and liver function tests compared with endoscopic retrograde cholangiography. Gastrointest Endosc 1996;44(2):158–63. [CrossRef]
[Pubmed]

16.
Ahmad NZ. Routine testing of liver function before and after elective laparoscopic cholecystectomy: Is it necessary? JSLS 2011;15(1):65–9. [CrossRef]
[Pubmed]

17.
Hayat JO, Loew CJ, Asrress KN, McIntyre AS, Gorard DA. Contrasting liver function test patterns in obstructive jaundice due to biliary strictures [corrected] and stones. QJM 2005;98(1):35–40. [CrossRef]
[Pubmed]

18.
Frossard JL, Hadengue A, Amouyal G, et al. Choledocholithiasis: A prospective study of spontaneous common bile duct stone migration. Gastrointest Endosc 2000;51(2):175–9. [CrossRef]
[Pubmed]

SUPPORTING INFORMATION
Acknowledgments
No preregistration exists for the reported studies reported in this article.
Author ContributionsBardia Bidarmaghz - Conception of the work, Design of the work, Acquisition of data, Analysis of data, Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Nestor Sabat - Conception of the work, Design of the work, Acquisition of data, Analysis of data, Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Aditya Sharma - Conception of the work, Design of the work, Acquisition of data, Analysis of data, Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Hugh McGregor - Conception of the work, Design of the work, Acquisition of data, Analysis of data, Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Jason Wong - Conception of the work, Design of the work, Acquisition of data, Analysis of data, Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Guarantor of SubmissionThe corresponding author is the guarantor of submission.
Source of SupportNone
Consent StatementWritten informed consent was obtained from the patient for publication of this article.
Data AvailabilityAll relevant data are within the paper and its Supporting Information files.
Conflict of InterestAuthors declare no conflict of interest.
Copyright© 2023 Bardia Bidarmaghz et al. This article is distributed under the terms of Creative Commons Attribution License which permits unrestricted use, distribution and reproduction in any medium provided the original author(s) and original publisher are properly credited. Please see the copyright policy on the journal website for more information.





/2023/images/figure1.jpg)
/2023/images/figure1.1669809768.jpg)
/2023/images/figure1.1669794569.jpg)
